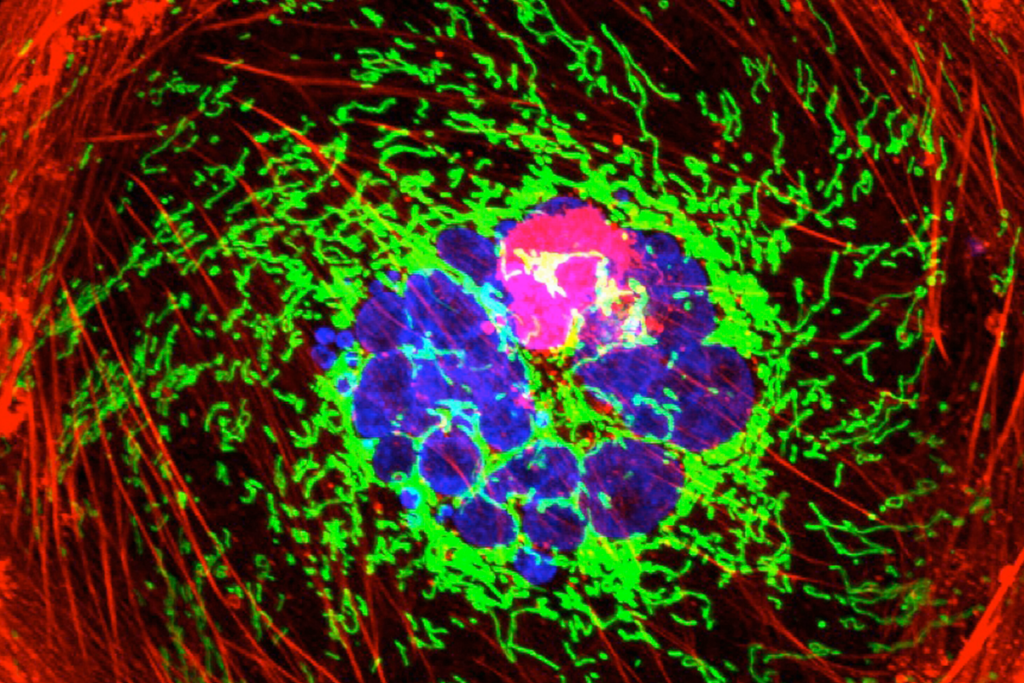
Tumors are characterized by the uncontrolled growth of cells, and there are over 100 different types of cancers, most of which are solid tumors. In some cases, solid tumors remain confined to the organ of origin (founder or primary tumor). However, cancer cells can acquire the ability to migrate and invade other tissues and organs, establishing new niches. Among the most common types are prostate, breast, cervical, lung, intestinal, stomach, and skin cancers.
Oncology advancements in recent decades have brought promising innovations in cancer treatment, particularly adoptive cell therapies (ACT) such as TIL, TCR-T, and CAR-T. By harnessing the immune system’s potential to identify and destroy tumor cells, this type of therapy represents a new frontier in precision medicine.
Developed by researcher Steven Rosenberg, a surgeon at the U.S. National Cancer Institute, starting in 1986, tumor-infiltrating lymphocyte (TIL) therapy involves extracting immune cells from the patient’s tumor. These cells, once cultured and expanded in the lab, are reintroduced into the body to attack cancer cells.
Simply put, TIL’s unique feature is its ability to recognize the unique neoantigens of each patient’s cancer. After recognizing the neoantigens, the TILs are activated and promote tumor destruction. According to this study, which analyzes the latest clinical research related to TIL, this personalized approach has shown higher response rates and better chances of remission.
How it works
TIL therapy involves extracting T and B lymphocytes directly from the patient’s tumor. Since these cells have already been exposed to the tumor and identified it as a foreign antigen, they can be isolated, expanded in the laboratory, and reintroduced into the body, targeting cancer cells precisely.
Because they are extracted from the tumor itself, TILs are personalized for each patient, significantly reducing the risk of rejection or graft-versus-host disease (GVHD), commonly associated with allogeneic therapies.
How it is used in solid tumors
According to this study, published on September 12, 2024, TIL therapy has shown promise in achieving long-lasting responses, even in advanced cancers or those with metastasis. Some patients have experienced complete and sustained remissions, suggesting that the treatment may offer long-term benefits.
Unlike CAR-T cell therapy, which has shown excellent results in hematological cancers, TIL therapy has been applied to a wide range of solid tumors, including melanoma, cervical cancer, lung cancer, breast cancer, and more recently, gastric intestinal cancer. This makes it a potentially valuable treatment option for a variety of cancer types.
Recently, the Food and Drug Administration (FDA) approved a TIL therapy called lifileucel (also known as Amtagvi) for the treatment of advanced melanoma, marking the first cellular therapy approved for treating solid tumors.
Additionally, TIL therapy can be used in combination with other immunotherapies, such as immune checkpoint inhibitors, to enhance its efficacy. This combined approach may provide additive or synergistic benefits in cancer treatment.
Side effects
As with any innovative therapy, there are potential risks and side effects. These may include transient dyspnea, chills, and fever shortly after infusion. However, these adverse effects are not associated with elevated cytokine levels in the blood and should not be confused with cytokine release syndrome, often seen in other cellular therapies like CAR-T.
More hope for cancer patients
With continuous advancements in biotechnology, several therapies, including TIL, are being optimized, bringing new hope to cancer patients. This study shows how medicine is evolving, intensely seeking new solutions for solid tumors. The future of precision medicine looks increasingly promising, with the possibility of more effective and personalized treatments for various types of cancer.
Also read our blog post “CAR Macrophages and CAR-T Cells: Combinatorial Immunotherapy.”